Why Do We Experience Phantom Limb Pain After Amputation?
Introduction
Phantom limb pain (PLP) is a perplexing phenomenon experienced by many amputees. Imagine a missing arm or leg, yet feeling sharp pains or tingles as if it were still there. This sensation isn’t just in their heads—it’s real and can significantly impact daily life. Research suggests that around 60% to 85% of amputees experience PLP. For many, this pain can be debilitating, disrupting their quality of life and hindering rehabilitation efforts.
Understanding why this occurs is crucial for better management and support for those affected. This article aims to shed light on the underlying causes of PLP, exploring the intricate connection between the brain, nerves, and the experience of pain in a limb that no longer exists.
Understanding Phantom Limb Pain
Phantom limb pain differs from other types of pain felt after an amputation. While residual limb pain arises from the remaining part of the limb, PLP occurs in the area where the limb once was. Patients may describe their experience as burning, tingling, or even severe stabbing sensations.
Approximately 60% to 85% of individuals report experiencing PLP, often within the first six months after amputation. Psychological factors play a pivotal role; stress, anxiety, and past pain in the limb can intensify sensations. Furthermore, the brain’s neural architecture adapts poorly to the loss, leading to misinterpretation of signals from the nervous system.
This phenomenon highlights the importance of addressing both psychological and physical aspects to effectively manage PLP. Understanding the nuances of PLP can help in developing targeted treatment strategies, thereby improving patient outcomes and overall quality of life.
For more insights into the complexities of phantom limb pain, it’s essential to explore why we experience this sensation after amputation. Why do we experience phantom limb pain after amputation
The Sensations of Phantom Limb Pain
Phantom limb pain manifests in various ways, often described as a complex mix of sensations. Common experiences include:
- Burning: This sensation can feel like a hot poker poking the nonexistent limb.
- Tingling: Often likened to “pins and needles,” it can be frustrating and uncomfortable.
- Aching: A persistent dull pain that can nag throughout the day.
- Stabbing: Sudden, sharp pains that can catch individuals off guard.
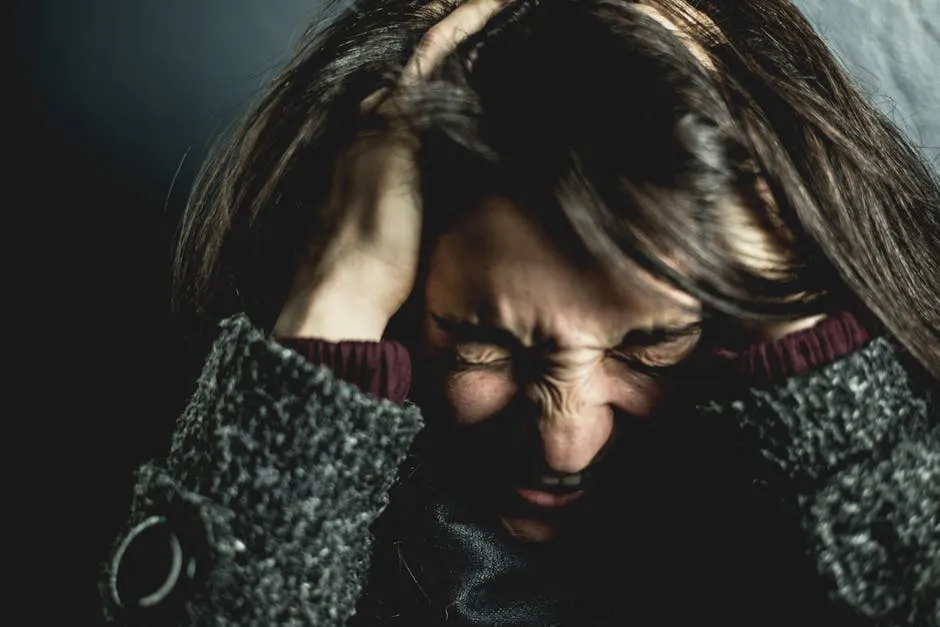
These sensations can have a significant psychological impact. For many, the perception of pain in a phantom limb can lead to feelings of frustration, anxiety, and helplessness. This emotional toll exacerbates the physical symptoms, creating a cycle that can be tough to break.
Understanding these sensations is key to developing effective coping strategies and treatments. By recognizing the range of experiences associated with PLP, healthcare providers can tailor their approaches to better address the unique needs of each individual.
Causes of Phantom Limb Pain
Phantom limb pain (PLP) is a complex phenomenon that arises after an amputation. While the exact reason behind this pain is still a puzzle, researchers have identified several mechanisms that contribute to its occurrence. One major factor is the way our nervous system adapts to the loss of a limb. After an amputation, the brain and spinal cord continue to receive signals from nerves that were previously connected to the missing limb. This miscommunication can lead to the sensation of pain, resulting in PLP.
Another important aspect involves the formation of neuromas. When nerves are cut during surgery, they can form painful growths known as neuromas. These neuromas can send erratic signals to the brain, causing the perception of pain in the absent limb. Additionally, changes in the brain’s structure and function after amputation play a crucial role. The brain may reorganize itself, leading to areas that used to receive input from the missing limb becoming hyperactive, which can further amplify the sensation of pain.
Psychological factors also contribute significantly to PLP. Individuals who experienced pain in their limb before the amputation are more likely to suffer from PLP afterward. Stress, anxiety, and depression can exacerbate the pain, making it even more challenging to manage. This combination of peripheral and central mechanisms, along with psychological influences, creates a multifaceted explanation for why PLP occurs. Understanding these causes is vital for developing effective treatments and support strategies for those affected.

Peripheral Mechanisms
During amputation, the nerves are inevitably damaged. This injury can lead to significant changes in how the body processes pain signals. When nerves are severed, they may not heal properly, leading to the formation of neuromas—benign growths that occur at the site of nerve injury. These neuromas can become overly sensitive, firing off painful signals to the brain even in the absence of stimulation. As a result, individuals may experience sharp, burning, or tingling sensations in their phantom limb.
Moreover, the altered nerve pathways can create an environment of heightened sensitivity. This phenomenon is known as peripheral sensitization, where nerve endings become more reactive due to changes in their structure and function. Such alterations can amplify the perception of pain, contributing to the discomfort associated with PLP.
Additionally, the body’s healing process may exacerbate the situation. Inflammation and scarring at the site of amputation can lead to further nerve irritation. As the residual limb undergoes healing, the signals sent from the nerves can become confused, leading to pain that feels like it originates from the absent limb. The interplay of these peripheral mechanisms highlights how crucial it is to focus on nerve health and management during the rehabilitation process for amputees.

Central Mechanisms
The brain plays a pivotal role in how we perceive pain. After an amputation, the areas of the brain that once processed sensory information from the limb may undergo significant changes. This phenomenon is referred to as cortical reorganization. When a limb is lost, the brain’s map of the body, known as the sensory homunculus, is altered. Neighboring areas of the cortex may take over the representations of the missing limb, potentially leading to misinterpretation of signals and the sensation of pain.
In addition, central sensitization occurs in the spinal cord and brain. This process involves an increase in the excitability of neurons, making them more responsive to stimuli. After amputation, the loss of input from the missing limb can cause the nervous system to become hyperactive, further contributing to the sensation of pain in the phantom limb. This heightened state of sensitivity can lead to PLP being triggered by non-painful stimuli or even spontaneously.
The interplay between cortical reorganization and central sensitization creates a complex environment where the brain is constantly trying to make sense of the signals it receives. This miscommunication can result in persistent pain and discomfort, emphasizing the need for targeted therapies that address both the physical and neurological components of PLP. Understanding these central mechanisms is crucial for developing effective pain management strategies for amputees.

Psychological Factors
Phantom limb pain (PLP) doesn’t just affect the body; it also messes with our minds. Imagine losing a limb and still feeling it nagging at you. For many amputees, this sensation is all too real. The psychological aspects play a significant role in how PLP manifests and evolves.
Pre-amputation pain can set the stage for PLP. Studies reveal that individuals who experienced pain in their limbs before amputation are more likely to report phantom pain afterward. It’s like your brain has a memory of the pain, and it just doesn’t let go. When the body experiences a sudden loss, the emotional toll can also contribute to heightened sensitivity to pain. Anxiety and stress become unwelcome companions, exacerbating the phantom sensations.
Stress, like a clingy friend, can amplify discomfort. When we’re anxious, our bodies respond with tension, which can heighten the perception of pain. This can create a vicious cycle; stress leads to pain, and pain leads to more stress. It’s a loop that many find frustrating.
Depression is another factor lurking in the shadows. The emotional fallout from losing a limb can weigh heavily on mental health. A low mood can make it harder to cope with any pain, phantom or otherwise. Individuals with depression may focus more on their discomfort, making it seem worse than it is.
Moreover, the brain’s adaptation to limb loss is a complicated affair. The brain doesn’t simply erase the map of the missing limb. Instead, it tries to make sense of the signals it receives. In this process, it can misinterpret these signals as pain. This cognitive dissonance between what the brain expects and what the body experiences can lead to a heightened perception of PLP.
Ultimately, addressing psychological factors is essential for managing PLP effectively. Therapeutic interventions, such as Cognitive Behavioral Therapy Workbooks, can help amputees process their feelings and develop coping strategies. By tackling the mental health challenges tied to PLP, individuals can find relief and improve their overall well-being.

Diagnosis of Phantom Limb Pain
Diagnosing phantom limb pain (PLP) is a crucial step in managing this complex condition. The process typically begins with a comprehensive medical history, where healthcare providers gather details about the patient’s amputation and any pre-existing pain. This conversation is key, as it sets the groundwork for understanding the individual’s experience.
Next up, the physical examination. Doctors assess the residual limb for any signs of infection or other complications. They might also evaluate how well the patient can move and feel in the remaining limb. This step is vital because it helps distinguish PLP from residual limb pain (RLP). While PLP occurs in the absent limb, RLP arises from issues in the remaining limb. Getting this distinction right is important for choosing the appropriate treatment.
In some cases, additional tests may be necessary. These could include imaging studies to rule out complications such as neuromas or infections. Blood tests might be conducted to check for underlying issues like inflammation.
Another valuable tool in diagnosing PLP is the pain diary. Patients are often encouraged to keep track of their pain patterns, noting when it occurs, the intensity, and any potential triggers. This record helps doctors gain a clearer picture of the patient’s experience, leading to more targeted approaches. A Pain Diary Journal can be incredibly helpful for this purpose.
Diagnosing PLP can be challenging due to the subjective nature of pain. No definitive test exists to confirm it. However, healthcare providers rely on the combination of medical history, physical examination, and patient-reported experiences.
Recognizing the difference between PLP and RLP is essential for effective treatment. Misdiagnosis can lead to inappropriate treatments, causing frustration for both patients and providers. By accurately diagnosing PLP, healthcare professionals can develop a tailored management plan that addresses the unique needs of each individual.

Treatment and Management of Phantom Limb Pain
Treating phantom limb pain (PLP) requires a multifaceted approach, as there’s no one-size-fits-all solution. The first step typically involves medication. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often used for initial pain relief. However, when PLP becomes more complex, doctors may prescribe antidepressants or anticonvulsants, known for their efficacy in managing nerve pain.
Another popular treatment option is transcutaneous electrical nerve stimulation (TENS). This method sends gentle electrical pulses through the skin, helping to disrupt pain signals. Many patients report finding some relief through TENS Units for Pain Relief, making it a go-to for managing PLP symptoms.
Mirror therapy has emerged as a fascinating way to address PLP. This technique tricks the brain into thinking the missing limb is still there. Patients look into a mirror that reflects their intact limb, creating the illusion of movement in the phantom limb. Research shows that this method can be surprisingly effective for some individuals, providing a bridge between the brain’s perception and the reality of limb loss.
Behavioral therapies also play a vital role in managing PLP. Cognitive-behavioral therapy (CBT) helps individuals cope with the emotional aspects of living with phantom pain. By addressing the psychological factors, patients can develop healthier responses to pain, reducing its perceived intensity.
For those with severe and persistent PLP, more invasive options may be considered. Spinal cord stimulation and other neuromodulation techniques have shown promise, especially for individuals who do not respond to traditional therapies. These methods work by altering the way pain signals are processed in the nervous system.
Ultimately, effective treatment requires a personalized approach. What works for one person may not work for another. A comprehensive pain management plan often includes a mix of medications, therapies, and lifestyle adjustments. By addressing both the physical and psychological aspects of PLP, individuals can find relief and improve their quality of life.

Medical Treatments
When it comes to managing phantom limb pain (PLP), a variety of pharmacological options can provide relief. Let’s take a closer look at some common medications used to tackle this perplexing pain.
NSAIDs (Nonsteroidal Anti-Inflammatory Drugs) are often the first line of defense. These over-the-counter heroes, like Ibuprofen Tablets and Naproxen Sodium Tablets, help reduce inflammation and alleviate mild pain. They may not completely banish PLP, but they can certainly take the edge off.
Next up are antidepressants, which might sound odd for pain management. However, medications like Amitriptyline Tablets and nortriptyline are frequently prescribed due to their ability to modulate nerve signals. Their effects can provide significant relief, especially for those experiencing neuropathic pain.
Anticonvulsants also play a vital role in this pain saga. Drugs such as Gabapentin Capsules and Pregabalin Capsules help stabilize nerve activity, reducing those pesky erratic pain signals. Many patients report a notable improvement in their symptoms when incorporating these medications into their regimen.
And let’s not forget about opioids. While they’re often reserved for more severe pain, medications like Morphine Pain Relief Medications can sometimes be prescribed for PLP. Caution is key here, as opioids come with the risk of dependency. Thus, they should be used judiciously and under close medical supervision.
In summary, managing phantom limb pain often requires a multifaceted approach involving various medications. Each individual may respond differently, so it’s essential to work closely with healthcare providers to find the most effective combination tailored to personal needs.

Non-Medical Therapies
In addition to medications, several complementary and alternative therapies can help alleviate phantom limb pain (PLP). These non-medical approaches may offer valuable relief and enhance overall well-being.
Mirror therapy is a fascinating technique gaining traction. By placing a mirror in front of the intact limb, patients can visualize the reflection as if they still have the missing limb. This clever trick can confuse the brain into perceiving movement in the phantom limb, often leading to reduced pain and discomfort. Consider using a Mirror Therapy Kit to get started!
Another popular option is TENS (Transcutaneous Electrical Nerve Stimulation). This method involves placing electrodes on the skin to deliver electrical impulses. These impulses can help interrupt pain signals before they reach the brain, offering a soothing effect. Many users find TENS units to be a handy tool for managing PLP on-the-go.
Acupuncture is yet another intriguing treatment. This ancient practice involves inserting thin needles into specific points on the body. It’s believed to stimulate the release of endorphins and other natural pain-relieving chemicals. Research shows that acupuncture can provide significant relief for some individuals suffering from PLP. You might want to look into Acupuncture Needles if you’re interested in trying it out!
Lastly, Cognitive Behavioral Therapy (CBT) can be beneficial in managing the emotional aspects of phantom limb pain. By addressing negative thought patterns and teaching coping strategies, CBT can help individuals navigate the mental challenges associated with PLP, ultimately leading to a more positive outlook and reduced pain perception.
Combining these therapies with medical treatments can create a holistic approach, empowering individuals to reclaim control over their pain and improve their quality of life.

Lifestyle Modifications
Lifestyle modifications play a crucial role in managing phantom limb pain (PLP). By incorporating certain practices into daily routines, individuals can experience relief and enhance their overall well-being.
Physical therapy is paramount. Engaging in targeted exercises can help strengthen the residual limb and improve mobility. A skilled physical therapist can develop a personalized program to address specific needs, making the transition to prosthetics smoother and more comfortable. Consider using Physical Therapy Resistance Bands to enhance your workouts.
Relaxation techniques are equally important. Practices such as deep breathing, yoga, and meditation can help reduce stress and anxiety, which are known triggers for PLP. By incorporating these techniques into daily life, individuals can foster a sense of calm, potentially alleviating some of the pain. A good Deep Breathing Exercise Guide can be a great addition to your routine.
Lastly, support groups offer a valuable resource. Connecting with others who share similar experiences can provide emotional support and practical advice. Knowing you’re not alone in this journey can be incredibly empowering and uplifting. You might even consider reading a Support Group Resource Book to guide you.
In conclusion, lifestyle modifications, including physical therapy, relaxation techniques, and support groups, can significantly impact the management of phantom limb pain. By taking a proactive approach, individuals can enhance their quality of life and navigate the complexities of PLP more effectively.

Living with Phantom Limb Pain
Living with phantom limb pain (PLP) can be a perplexing experience. One moment, you’re feeling fine, and the next, a wave of pain hits you in a limb that’s no longer there. Many amputees report these sensations, which can vary from mild tingling to intense, stabbing pain. Managing everyday life with PLP requires a multifaceted approach, combining physical and emotional strategies.
First, understanding your pain is crucial. Many people find that keeping a pain diary helps them track when the pain occurs and what might trigger it. This can be beneficial for both patients and healthcare providers. It allows for a clearer understanding of patterns, making it easier to develop effective coping strategies.
Coping strategies can be as varied as the sensations themselves. For some, engaging in physical therapy helps. Gentle exercises can strengthen the residual limb and improve overall mobility. Moreover, practicing relaxation techniques—such as deep breathing or yoga—can help quell anxiety that often exacerbates PLP. Stress management is essential; when you’re under pressure, your pain can feel more intense.
Mental health support plays a significant role in coping with PLP. Joining a support group can provide a sense of community. Sharing experiences with others who understand can reduce feelings of isolation. Therapists specializing in chronic pain management can also aid in addressing underlying emotional challenges.
One innovative approach is mirror therapy. This technique involves using a mirror to reflect the intact limb, creating an illusion that the phantom limb is still present. Patients often report a reduction in pain after engaging in this visual trickery. It’s fascinating how our brains interpret sensory information!
Incorporating mindfulness practices can also be beneficial. Techniques like meditation or guided imagery can help you focus on positive sensations rather than pain. This shift in focus can reduce the intensity of phantom sensations and promote a more relaxed state.
Overall, managing phantom limb pain is about finding what works best for you. A combination of physical, mental, and emotional strategies can significantly improve quality of life. Remember, it’s perfectly okay to seek help from healthcare professionals, as they can provide tailored support.

Conclusion
Phantom limb pain (PLP) is a complex phenomenon that many amputees face. Understanding the nature of this pain is essential for effective management and support. We’ve explored how PLP can manifest, the underlying causes, and the strategies to cope with it.
Recognizing the psychological aspects of PLP is crucial. Stress, anxiety, and past pain in the limb can exacerbate the sensations experienced. By addressing these factors through mental health support, amputees can improve their quality of life.
Continued research into phantom limb pain is vital. A deeper understanding of its mechanisms can lead to better treatments and support for those affected. It’s essential to encourage ongoing dialogue and awareness about PLP, ensuring that amputees receive the help they need.
If you or someone you know is struggling with PLP, know that you’re not alone. Support networks, healthcare providers, and innovative therapies are available to help navigate this challenging experience.
FAQs
What percentage of amputees experience phantom limb pain?
Research indicates that approximately 60% to 85% of amputees experience phantom limb pain at some point after their amputation.
How long does phantom limb pain typically last?
The duration of phantom limb pain varies widely among individuals. Some may experience it for a few months, while others may have persistent pain that lasts for years.
Are there any preventive measures for phantom limb pain?
While there is no guaranteed way to prevent phantom limb pain, some studies suggest that using both spinal and general anesthesia during surgery may reduce the risk.
Can phantom limb pain go away over time?
Many individuals report a decrease in the intensity and frequency of phantom limb pain over time. However, some may continue to experience it long-term.
What should I do if I experience phantom limb pain?
If you experience phantom limb pain, it’s essential to consult with a healthcare provider. They can help develop a personalized management plan that may include medication, therapy, or alternative treatments.
Please let us know what you think about our content by leaving a comment down below!
Thank you for reading till here 🙂
All images from Pexels